LONDON (TIP): A 22-year-old man charged with the murder of a 66-year-old Indian-origin woman as she waited at a bus stop in north-west London has been remanded in custody at a hearing on Tuesday, May 14.
Anita Mukhey, who worked part-time for the National Health Service (NHS) as a medical secretary, was waiting at the Burnt Oak Broadway bus stop in the Edgware area of London last week when Jalal Debella is accused of fatally stabbing her in the chest and neck. He appeared at Old Bailey Court in London and will enter his plea of guilty or not guilty at the next hearing in the case scheduled for August.
“Police were called around 11.50 am on Thursday, May 9, to reports of a stabbing in Burnt Oak Broadway,” Metropolitan Police said.
“Officers, London Ambulance Service (LAS) and London’s Air Ambulance (HEMS) all attended the scene, where a 66-year-old woman was treated for knife wounds. Sadly, despite the best efforts of emergency services, she died at the scene. Her family have been informed,” the police said.
Debella was arrested on suspicion of murder in the Colindale area of north London later on May 9 and charged with Mukhey’s murder and also for possession of an offensive weapon. The Crown Prosecution Service (CPS) told the court that a preliminary cause of death was found to be sharp force injuries to the front of the chest and neck.
“Anita Mukhey, 66 years old, was a married mother and grandmother devoted to her family, who also worked part-time in the NHS as a medical secretary. The family ask for privacy at this difficult time,” Mukhey’s family said in a statement issued via the police.
According to reports, members of the public screamed and shouted at the suspect to stop as the daylight attack sent shockwaves across the community.
Tag: NHS
-

Indian-origin woman stabbed to death at a bus stop in London
-

Indian-origin neurologist Dr Ashvini Keshavan’s UK study to revolutionize dementia diagnosis
LONDON (TIP): An Indian-origin neurologist is part of a world-class research team in the UK that has been awarded a major grant this week to build on recent breakthroughs in potential dementia blood tests and generate the evidence needed for them to be used more widely in the next five years.
Dr Ashvini Keshavan, Senior Clinical Research and Honorary Consultant Neurologist Fellow at University College London (UCL) is part of the team that will focus on the most promising biomarker for Alzheimer’s disease called p-tau217. A second team made up of researchers from the Universities of Oxford and Cambridge will test various proteins to detect a variety of dementia-causing diseases.
Both teams will recruit participants from sites spread across the UK with the hope of its cost-effective rollout on the National Health Service (NHS) over time.
“Proteins that underpin various dementia-causing diseases, and particularly Alzheimer’s disease, which is the commonest cause of dementia worldwide, are now detectable in blood,” said Dr Keshavan.
“The two studies that have been awarded funding by the Blood Biomarker Challenge grant are both seeking to implement blood tests in real world settings in the UK, to see if blood tests will prove useful in confirming the presence or absence of these diseases in people who have early dementia or mild but progressive cognitive problems. We want to ensure that our research will reflect the UK’s ethnic and socioeconomic diversity and are aiming to broaden access to these tests, as the current gold standard tests to confirm the presence of these diseases are currently not accessible to most UK patients because they are either expensive or invasive,” she explains.
The Blood Biomarker Challenge is a multi-million-pound award given by Alzheimer’s Society, Alzheimer’s Research UK, the UK’s National Institute for Health and Research and Gates Ventures and includes funds raised by players of People’s Postcode Lottery.
The UCL-led study is called ADAPT and will focus on plasma p-tau217 – a blood marker of Alzheimer’s disease – and will answer the question of whether knowledge of this test result can improve rates of Alzheimer’s diagnosis in conjunction with standard memory clinic assessments. The second study is called READ-OUT, which aims to test various proteins, including novel or less well-established ones, to detect a variety of dementia-causing diseases.
“If our research shows that these tests are clinically useful, and cost-effective, we would be able to contribute to the case for them becoming a part of the standard of care offered in the UK. This would have the potential for individuals to receive earlier diagnoses of their specific dementia-causing disease,” said Dr Keshavan.
Such a breakthrough would be particularly important for ensuring patients are given the right post-diagnostic support and treatment for symptoms.
“An early, accurate diagnosis of Alzheimer’s disease is already important, allowing people to access appropriate care and medications. If, as we hope, new treatments that can slow down Alzheimer’s disease become available soon, then this will be vital. This would pave the way for fair and equitable access to new and potentially life-changing treatments to all who might benefit,” added Professor Jonathan Schott, Alzheimer’s Research UK Chief Medical Officer and Dr Keshavan’s UCL colleague on the research.
Currently, people are usually diagnosed with dementia using memory tests and brain scans. These are less accurate than “gold standard” tests like PET scans or lumbar punctures, which can confirm what type of dementia they have. However, only 2 per cent of people can access these specialist tests.
In recent years, several different blood tests that can diagnose Alzheimer’s disease and other causes of dementia have shown very promising results in research settings. But they have yet to be tested widely in clinical settings in the UK.
Dr Vanessa Raymont, Associate Director, Dementias Platform UK, and Senior Clinical Researcher, University of Oxford, said: “There was previously a feeling that this was just another part of aging, but now we’re seeing that people want to know more about their condition, and they want a diagnosis as it helps them access the support they need.
“Both my parents lived with dementia so I know first-hand the devastation this disease causes, and how a timely and accurate diagnosis can benefit people and their families.” Blood tests are seen as part of the answer to addressing the dementia conundrum as they’re quick, easy to administer and cheaper than current, more complex tests. -

Indian-origin medic Meghana Pandit named CEO of Oxford University Hospitals
LONDON (TIP): Professor Meghana Pandit, a leading Indian-origin medic was appointed the chief executive officer (CEO) of the Oxford University Hospitals NHS Foundation Trust, one of the UK’s largest teaching hospitals.
Pandit becomes the trust’s first female chief, and she is also the first person of Indian heritage to be appointed CEO of any National Health Service (NHS) trust in the Shelford Group, which represents some of the biggest teaching hospitals in the country.
Pandit, who was serving as the interim CEO at Oxford University Hospitals (OUH) since July 2022, was permanently appointed to the post following a “rigorous and competitive process,” which concluded after what OUH described as an extensive national and international recruitment search.
“It is a privilege to be asked to lead OUH on a permanent basis and I look forward to continue working with colleagues at OUH, our partners in the health and social care system in Oxfordshire and across the BOB Integrated Care System, our partner universities, and Oxford Hospitals Charity, to ensure the highest quality of research and innovation enabled care for our patients and populations,” said Pandit.
“I am proud to have the opportunity to continue leading with compassion and respect for others, with a desire for excellence,” she said.
Pandit got trained in Obstetrics and Gynecology in the Oxford Deanery and was a visiting lecturer in Urogynecology at the University of Michigan in the US.
She has served as Chief Medical Officer (CMO) within the NHS trusts and led the development of a clinical strategy with the responsibility of overseeing hundreds of doctors.
She is an Honorary Professor at Warwick University and an Associate Fellow at Green Templeton College, University of Oxford.
According to OUH, all members of the interview panel unanimously agreed that she was the preferred candidate for appointment and this recommendation was approved at a meeting of the Council of Governors earlier this week.
The interview panel included the Trust’s Chair, Professor Sir Jonathan Montgomery, two other non-executive directors and lead governor, and also the chair of the Buckinghamshire, Oxfordshire and Berkshire West Integrated Care Board (BOB ICB) and the Regional Director for NHS England’s Southeast region.
“I am delighted that Meghana has now been appointed to the CEO role on a permanent basis and I am looking forward to working with her personally in what promises to be an exciting new era under her leadership,” said Montgomery. “She gave an outstanding interview which demonstrated her preparation, passion, and desire to take on the role of Chief Executive Officer on a permanent basis,” Montgomery said.
Meghana has a strong focus on staff engagement and building the patient voice into the strategic development of the Trust and her approach is strongly aligned with our trust values and with our vision of delivering compassionate excellence to our patients,” he said.
The CEO of the NHS trust is personally responsible, along with the NHS Chief Executive, as the parliamentary accountable officer for ensuring that the organization works effectively in accordance with national policy and public service values and maintains proper financial stewardship.
The CEO is also personally accountable for clinical governance and partnerships. -

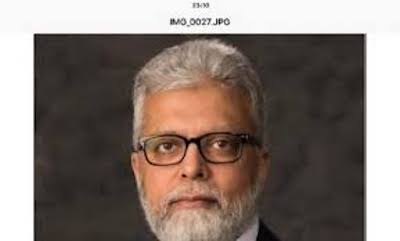
Leading Indian-origin doctor Ranjit Manchanda to chair AIIMS Infosys Oncology
LONDON (TIP): Leading India-origin gynecological oncologist Ranjit Manchanda from London’s Cancer Research UK Barts Centre has bagged the prestigious Infosys Chair in Oncology at All India Institute of Medical Sciences, New Delhi. Manchanda, an alumnus of AIIMS New Delhi, completed his MBBS and MD from AIIMS in 1990s before proceeding to the University College London, UK for PhD in gynecological oncology. An acclaimed super specialist, Manchanda’s research spans targeted precision prevention of cancer. His core work includes population-based germ line testing for risk prediction, targeted screening and cancer prevention; developing targeted surgical prevention strategies for ovarian and endometrial cancer; developing genetic testing strategies as cancer diagnosis and prevention and management of familial gynecological cancer.
Currently Professor, Gynecological Oncology at the Wolfson Institute of Population Health at Queen Mary University of London and Consultant Gynecological Oncologist at Barts Health National Health Services Trust, Manchanda is leading several crucial research projects, early detection of ovarian cancer among them.
“This award means a lot to me and it is an honor and privilege to have received it. I am excited at the opportunity to work with colleagues at AIIMS across both clinical and academic domains, and bring our institutes together with the common aim to reduce the burden of disease and improve the lives of women affected by gynecological cancer,” Manchanda said. His work at Infosys Chair will support the division of Gynecological Oncology at AIIMS and will grow collaborative working between Queen Mary University of London, Barts Health NHS Trust and AIIMS.
It will aid early screening strategies for ovarian cancer, the second most common gynecological cancer in India and a leading cause of death from cancer in Indian women with 3.34 per cent (24,015) of cancer deaths in one year.
Advanced ovarian cancer has a dismal prognosis, with the highest case fatality ratio amongst all gynecological cancers globally – which explains the criticality of Manchanda’s expertise in the area.
While 5-year survival from ovarian cancer is 94 per cent when diagnosed in Stage I, only 15 per cent cases are diagnosed at this stage. Most (62 per cent) of cases are diagnosed in Stages III and IV, when 5-year survival is only 28 per cent. Manchanda was previously Director Graduate Studies, Wolfson Institute of Population Health, Queen Mary University of London and Clinical Senior Lecturer, Barts Cancer Institute, Queen Mary University of London.
He has several top awards to his credit including Columbia Hospital for Women Research Foundation Award for the most impactful paper in 2020-21, NHS Innovation Accelerator NIA Fellowship and the William Blair Bell Memorial Lecture Award of the Royal College of Obstetricians and Gynecologists.
-
Third lockdown begins in UK, stay-at-home order till mid-February
London (TIP): Britain began its third Covid lockdown on Tuesday with citizens under orders to stay at home and the government calling for one last major national effort to stem the virus before mass vaccinations turn the tide. Finance minister Rishi Sunak announced a new package of business grants worth 4.6 billion pounds ($6.2 billion) to help keep people in jobs and firms afloat until measures are relaxed gradually, at the earliest from mid-February but likely later. Britain has the second highest death toll in Europe. Its economy suffered the sharpest contraction of any in the Group of Seven during the first wave of infections last spring.
PM Boris Johnson announced the new lockdown late on Monday, saying the highly contagious new Covid variant first identified in Britain was spreading so fast the National Health Service (NHS) risked being overwhelmed within 21 days. In England alone, some 27,000 people are in hospital with Covid, 40% more than during the first peak in April, with infection numbers still expected to rise further after increased socialising during the Christmas period.
A Savanta-ComRes poll taken just after Johnson’s address suggested four in five adults in England supported the lockdown. Since the start of the pandemic, more than 75,000 people have died in the United Kingdom within 28 days of testing positive, according to official figures. — Reuters -
Indian-Origin Pathologist Accused of Bungling Post-Mortem Reports in UK
LONDON(TIP): Indian-origin pathologist, Khalid Ahmed, has been accused of mis handling some post-mortems at a UK hospital and is under police investigation to establish if any criminal charges need to be brought against him. Ahmed, who worked as a consultant pathologist at the Royal Oldham Hospital in Manchester, carried out an undisclosed number of post-mortem tests for the north Manchester coroner’s office.
An investigation revealed that he repeatedly recorded the wrong cause of death for patients, misidentified organs and potentially mixed up bodies, The Daily Telegraph reported.
In May last year, the senior coroner at the north Manchester coroner’s office raised concerns about Khalid Ahmed’s examinations and a recent review found “significant concerns” with his “inadequate” said reports.
Professor Simon Kim Suvarna, a consultant histopathologist at Sheffield Teaching Hospitals, carried out the review into Ahmed, who qualified as a medic in Bengaluru in 1989, and found some reports to have an “incorrect” cause of death given.
Suvarna is also reported to have noted that Khalid Ahmed’s tests “do not even meet the standards that are expected for pathology students to pass the autopsy component of the final exam”, the reports said.
A subsequent police referral was made by the coroner and that the police investigation is still underway.
A spokesperson for Greater Manchester Police (GMP) said: “GMP is assessing what, if any, criminal offences may have been committed in relation to findings presented to the coroner.”
Khalid Ahmed joined Pennine Acute NHS Trust in January 2007, but no longer works there.
In a statement, the trust said after they were told of the coroner’s concerns, an “in-depth internal review” into Khalid Ahmed’s practice was carried out, which concluded in February this year.
The trust added that a “thorough and extensive investigation” of Ahmed’s work for the UK’s state-funded National Health Service (NHS) work “provided assurance” his practice was “within the range of a reasonable pathologist”.
The UK’s General Medical Council said he is still licensed to practice as a histopathologist.