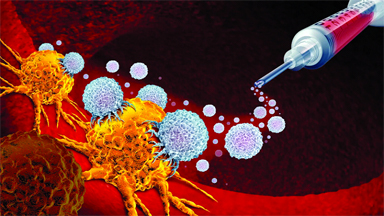
The Korea Advanced Institute of Science and Technology (KAIST) researchers have developed a way to reprogram immune cells already inside tumours into cancer-killing machines. A drug injected directly into the tumour is absorbed by macrophages, prompting them to recognise and attack cancer cells while activating nearby immune defences.
This eliminates the need for lab-based cell extraction and modification. In animal models, the strategy significantly slowed tumour growth and sparked strong anticancer immune responses.
KAIST (President Kwang Hyung Lee) announced that a research team led by Professor Ji-Ho Park from the Department of Bio and Brain Engineering has developed a new treatment approach.
When a drug is injected directly into a tumour, macrophages already present in the body absorb the drug and begin producing CAR (a cancer-recognising device) proteins. This process converts them into anticancer immune cells known as “CAR-macrophages.”
Solid tumours, including gastric, lung, and liver cancers, form dense structures that block immune cells from entering or functioning effectively because of this physical and biological barrier, many existing immune cell therapies struggle to work well against these types of cancers.
CAR-macrophages have emerged as a promising next-generation immunotherapy. Unlike some immune cells, macrophages can directly engulf and destroy cancer cells. They also stimulate nearby immune cells, helping to amplify the body’s overall anticancer response.
Despite their potential, current CAR-macrophage therapies rely on extracting immune cells from a patient’s blood, growing them in the lab, and genetically modifying them before reinfusion. This process is slow, expensive, and difficult to scale, which limits its practicality for many patients.
To bypass these challenges, the KAIST team focused on “tumour-associated macrophages” that naturally gather around tumours. The researchers developed a method to reprogram these cells directly inside the body rather than modifying them outside it.
Their approach uses lipid nanoparticles — engineered to be easily taken up by macrophages — loaded with both mRNA that carries cancer-recognition instructions and an immune-activating compound.




Be the first to comment